Regenerative medicine is advancing—yet systems still fail to catch the breakdown in progress.
While Science Builds the Future, the Body Keeps Breaking
The Frontier of Medicine Moves Fast
Two major stories this week show just how far science is pushing the boundaries of what the human body can recover from—and what it might soon be able to replace entirely. These breakthroughs reflect how rapidly medical innovation is evolving—but they also raise a deeper question: who will benefit from this progress, and who is still left behind?
A Paralyzed Man Walks Again

Source : Nature
A Japanese man with paralysis can now stand on his own after receiving an injection of neural stem cells derived from reprogrammed (iPS) cells — part of a first-of-its-kind clinical trial led by scientists at Keio University in Tokyo. Of the four men treated, two showed improvement, with one gaining the ability to move limbs and the other able to stand independently. The other two showed no significant recovery.
The trial used donor-derived iPS cells that were converted into neural precursors and injected into the spinal injury site. The team observed no serious side effects after one year.
Although the trial wasn’t designed to prove effectiveness, it represents a hopeful step toward using stem cells for spinal cord injury treatment. The idea of leveraging stem cells is central to how many scientists aim to address aging at the cellular level.
“Spare” Human Bodies
Source : MIT Technology Review
At Stanford, scientists have proposed creating sentience-free, lab-grown human bodies—referred to as “bodyoids“—using pluripotent stem cells, artificial wombs, and genetic techniques that inhibit brain development. These bodyoids would lack consciousness or the capacity to feel pain, making them ethically distinct from viable human beings.
Though still theoretical, this concept is gaining attention because it could help address major challenges in medicine: organ shortages, the ethical limits of animal testing, and the cost and speed of drug development.
Body replacement is also an active area of interest in anti-aging research, where one vision for solving aging involves gradually replacing parts of the body—or even the entire body, except for the brain—with engineered equivalents. Some even imagine progressive brain replacement as a future extension of this concept.
While current technologies make this vision plausible, the ethical stakes are high. Concerns include consent around donor cells and the risk of blurring the line between human and non-human forms.
As noted in our previous issue, there’s a growing call to action around the societal readiness for longevity and augmented human technologies. These discussions are no longer theoretical—they’re increasingly urgent.
And Then—Reality Reminded Us
Where We Still Are

Just as these headlines were making waves, a real-world loss brought us back to the present.
Han Jong-Hee, Vice Chairman and CEO of Samsung Electronics, collapsed from a heart attack during his daughter’s wedding and passed away the next day at the age of 63—just five days after standing on stage at an investor session, publicly addressing the company’s underperformance.
Executives like Han receive top-tier medical screenings annually, often with extensive diagnostics and customized care. Yet none of it was enough. No alert. No warning. No intervention.
This wasn’t an issue of access. It was a failure to sense the decline before the break—a blind spot our current healthcare system still doesn’t know how to see.
It Wasn’t About Access. It Was About Awareness.
Han didn’t suffer from a lack of care. Perhaps he felt tired at times, but without any diagnosis or alarming results, he likely believed he was still fine—just under pressure, like always.
Our systems are designed for DISEASE CARE, not HEALTH PRESERVATION. No incentives exist for catching dysfunction early. No metrics reward staying well. And no one owns the grey zone between “not yet sick” and “already too late.”
Even as we design synthetic organs, we still miss the opportunity to protect the bodies we already have.
The Shift from Sickcare to Healthcare
Has Already Begun
Medical progress means nothing if we only act after the damage is done.
Thankfully, over the past two decades, aging science has made significant progress in understanding how the body declines—revealing patterns that are measurable and, increasingly, modifiable.
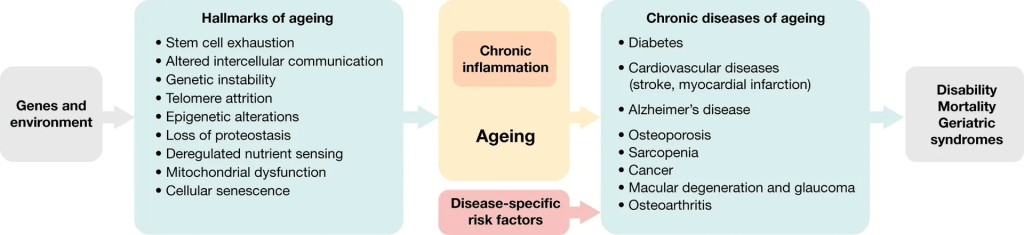
Until now, those insights lived apart from the mainstream healthcare system—partly because they didn’t align with traditional reimbursement models or short-term clinical goals, and partly because accountability for preventive outcomes is fragmented across stakeholders, with no single entity owning the long-term trajectory of health.
That’s beginning to change.
Public awareness is growing—fueled by data-driven insights into biological aging and the rising visibility of preventive strategies that can slow decline and extend function. This shift has been accelerated by pioneering researchers, longevity professional influencers, and therapeutic breakthroughs like GLP-1. Even in politics, preventive care is gaining traction.
The future of medicine won’t be defined by what we can fix—it will be measured by how early we can intervene, how long we can preserve function, and how well we can keep people from becoming patients in the first place.
Preventive care isn’t just the next chapter. It’s the foundation of a healthcare system that works.

Leave a comment